Researchers in Denmark conducted a study to investigate the impact of PrEP on sexually transmitted infections (STIs). The study monitored individuals attending sexual health clinics, tracking their diagnoses of three common bacterial STIs - chlamydia, gonorrhea, and syphilis - both before and after they began taking PrEP.
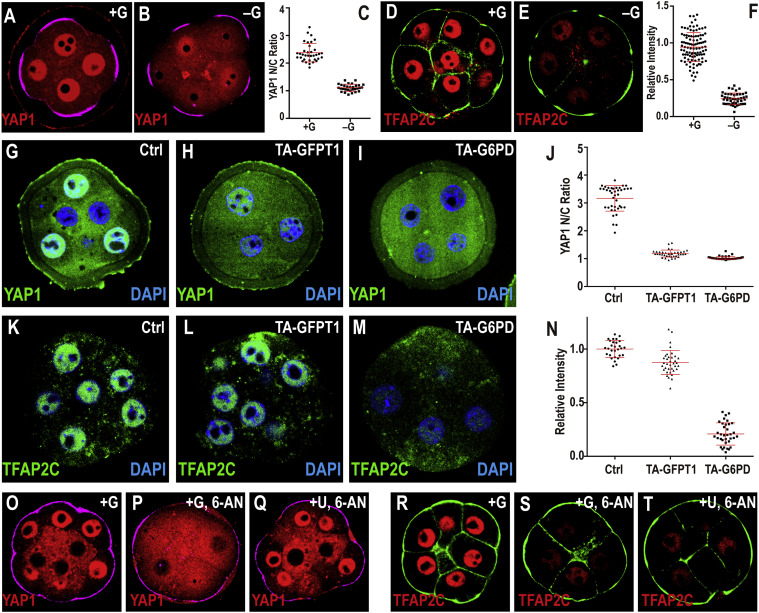
The initial findings seemed concerning, revealing that participants had more than twice the number of STI diagnoses (a 115% increase) while on PrEP compared to the period before starting it. However, a deeper analysis revealed a crucial factor: this significant rise was primarily driven by a substantial increase in STI testing frequency. Before starting PrEP, the average testing rate was around 50 tests per 100 person-years, which translates roughly to a test every two years. In contrast, individuals on PrEP received significantly more frequent testing, averaging three to four tests per year, with peaks in testing coinciding with their regular PrEP checkups every three months.
Taking this increased testing into account painted a different picture. When adjusted for testing frequency, the actual STI rate among those on PrEP only showed a 35% increase compared to the pre-PrEP period. Interestingly, the study found no significant rise in syphilis diagnoses specifically after starting PrEP.
In essence, the initial surge in STI diagnoses among PrEP users wasn't necessarily indicative of a dramatic increase in infections. The more frequent testing associated with PrEP programs played a major role in identifying existing STIs that might have otherwise gone undetected. While a moderate actual increase in STI rates was observed after adjusting for testing, the study also highlighted that syphilis diagnoses remained stable.
The study unearthed a surprising trend: Instead of a spike in STI testing only after starting PrEP, the researchers observed a gradual increase in tests during the months leading up. This suggests people weren't waiting to feel protected by PrEP before getting checked for STIs, which directly contradicts the theory of "risk compensation."
Let's break down risk compensation: It's the idea that adopting one protective measure (like PrEP for HIV) might lead people to engage in riskier sexual behaviors (like skipping condoms) because they feel a false sense of security. With PrEP's arrival, some researchers worried this could lead to a rise in STIs.
This study challenges that notion. The steady increase in STI testing before PrEP use indicates that people weren't becoming less cautious about their sexual health. The authors point out that if risk compensation were truly at play, a significant jump in STI rates would be expected immediately after starting PrEP, not before. This observed pattern suggests a more responsible approach – people might be taking PrEP as an additional layer of protection while still maintaining safe sex practices and getting tested regularly.
Here's an expanded version that dives deeper into the challenges of studying risk compensation with PrEP:
The Puzzle of PrEP and Risky Behavior
Figuring out if PrEP use leads to riskier sexual behavior is a complex question. Ideally, researchers would track individuals' STI history before they start PrEP. But gathering this complete picture is tricky for a few reasons.
Incomplete Data: Researchers often rely on medical records after someone starts PrEP. This lack of pre-PrEP STI information makes it difficult to establish a clear baseline.
Testing Bias: PrEP users tend to get tested for STIs more frequently. This increased testing can identify more infections, particularly those without symptoms. For example, studies estimate that a staggering 85% of rectal chlamydia and gonorrhea infections in gay men go unnoticed. This means a rise in STI diagnoses after PrEP use might not necessarily reflect increased risky behavior, but rather the detection of previously undiagnosed infections.
Further complicating the picture, some studies suggest STI diagnoses or riskier sexual behavior might actually have been higher before men started PrEP. This contradicts the initial concern about PrEP leading to increased risk. On the other hand, some studies do show higher STI rates after PrEP initiation. This is why further research is needed, as explored in detail within an aidsmap report on PrEP and STIs.
Denmark's meticulous healthcare system provides the perfect environment for this robust study. Each citizen has a unique ID that connects them to comprehensive databases of medical test results. This minimizes the chance of data getting lost in the system, ensuring a clearer picture.
PrEP and the DanPrEPD Study: Since 2018, anyone starting PrEP through the Danish public health system is automatically enrolled in the DanPrEPD study, regardless of whether they continue taking PrEP. This particular study focused on all transgender individuals and cisgender gay men who initiated PrEP between 2019 and 2022 in the Capital Region, a zone encompassing 30% of Denmark's population.
Participant Demographics: A total of 1,326 people participated, with 10 identifying as transgender. The average age was 35, with participants ranging from 16 to 78 years old. Nearly all (1,318) began taking daily PrEP. To ensure a more accurate comparison of pre- and during-PrEP experiences, some adjustments were made. This involved excluding 147 individuals who were already using PrEP before 2019. Additionally, 237 participants who stopped taking PrEP during the study were taken out of the analysis (although there may be some overlap if they were also part of the pre-2019 group).
Balanced Data Collection: The remaining participants, those who started and continued PrEP throughout the study, provided a well-balanced dataset. The researchers were able to analyze roughly the same amount of data from both periods: 2,155 person-years of data before starting PrEP and 2,351 person-years after. On average, there was a 22-month gap between entering the study and starting PrEP, with the entire study spanning 42 months. This even distribution allows for a more reliable comparison of health outcomes before and after initiating PrEP.
The study identified a significant rise in diagnosed STIs among participants after they began taking PrEP. The number of diagnoses jumped from 708 before PrEP to 1849 afterward. It's important to remember, however, that this doesn't automatically translate to everyone on PrEP getting an STI. The increase likely reflects more frequent STI testing, potentially due to heightened awareness or healthcare provider recommendations while on PrEP.
However, even accounting for potential testing changes, the study found a substantial increase in the rate of diagnosed STIs. This rate, expressed as an Incidence Rate Ratio (IRR), was over 2 times higher after starting PrEP compared to before (2.15 times more frequent). Notably, this rise wasn't limited to just one type of STI, but was observed across all the STIs included in the study.
More Testing, Not Just More Infections:
People on PrEP got tested for STIs much more frequently: nearly three times as many tests (23,654) compared to before (7,936).
This jump was especially high for syphilis (4.4 times more tests) because the test became routine, unlike the pre-PrEP period where it was only done half the time.
Adjusting for Increased Testing:
When researchers considered the extra testing, the actual increase in STI diagnoses dropped significantly.
The overall increase in STIs went from doubling (IRR 2.15) to just a 35% rise (IRR 1.35). Similar trends were seen for individual STIs.
Where Might Asymptomatic Infections Be Hiding?
Certain locations like the rectum have a higher rate of asymptomatic chlamydia compared to others (throat, genitals).
Conversely, most urethral gonorrhea infections show symptoms, unlike rectal or throat infections.
This suggests that if PrEP is leading to more diagnoses of asymptomatic infections, the increase might be higher for rectal chlamydia and lower for urethral gonorrhoea compared to other locations.
This rephrasing aims to:
Simplify the language.
Highlight the key points: increased testing and its impact on IRR.
Explain the potential link between testing location and asymptomatic infections.
The Rise in Diagnosed STIs with PrEP: Finding More Infections, Not Necessarily Causing Them
The study observed an increase in diagnosed STIs among people who recently began taking PrEP. However, this doesn't necessarily mean PrEP itself caused them to get more infections. Here are two main explanations:
PrEP Targets Those at Higher Risk: People with a higher risk of contracting STIs are more likely to choose PrEP as a preventative measure. So, the observed rise in diagnoses could simply reflect that PrEP is being used effectively by the population most susceptible to these infections.
Increased Testing Uncovers Hidden Infections: Regular testing is a crucial part of PrEP care. This more frequent testing can detect asymptomatic infections that would have otherwise gone unnoticed before starting PrEP. Essentially, PrEP doesn't create new infections, it improves the detection of existing ones.
Testing Frequency Makes a Difference: Catching Asymptomatic Infections
The study also revealed that the increase in diagnosed STIs was primarily due to asymptomatic infections. This highlights the importance of regular testing in catching infections that wouldn't cause noticeable symptoms. PrEP itself doesn't directly increase the number of infections, but the increased testing associated with PrEP care helps identify hidden cases.
PrEP Doesn't Encourage Risky Behavior, It Fills a Need for Protection
The researchers emphasize that PrEP doesn't lead people to engage in riskier sexual behavior. Instead, it's likely that people who already have a higher risk of STIs are opting for PrEP as a protective measure. This finding underscores the importance of PrEP for these individuals who are most vulnerable to infections.
PrEP Programs: A Platform for Promoting Safe Sex Practices
Since regular healthcare visits are part of PrEP use, it creates a valuable opportunity for open discussions about safe sex practices. This allows healthcare providers to address any concerns and provide guidance on how to further reduce the risk of STIs alongside PrEP use.






















0 Comments