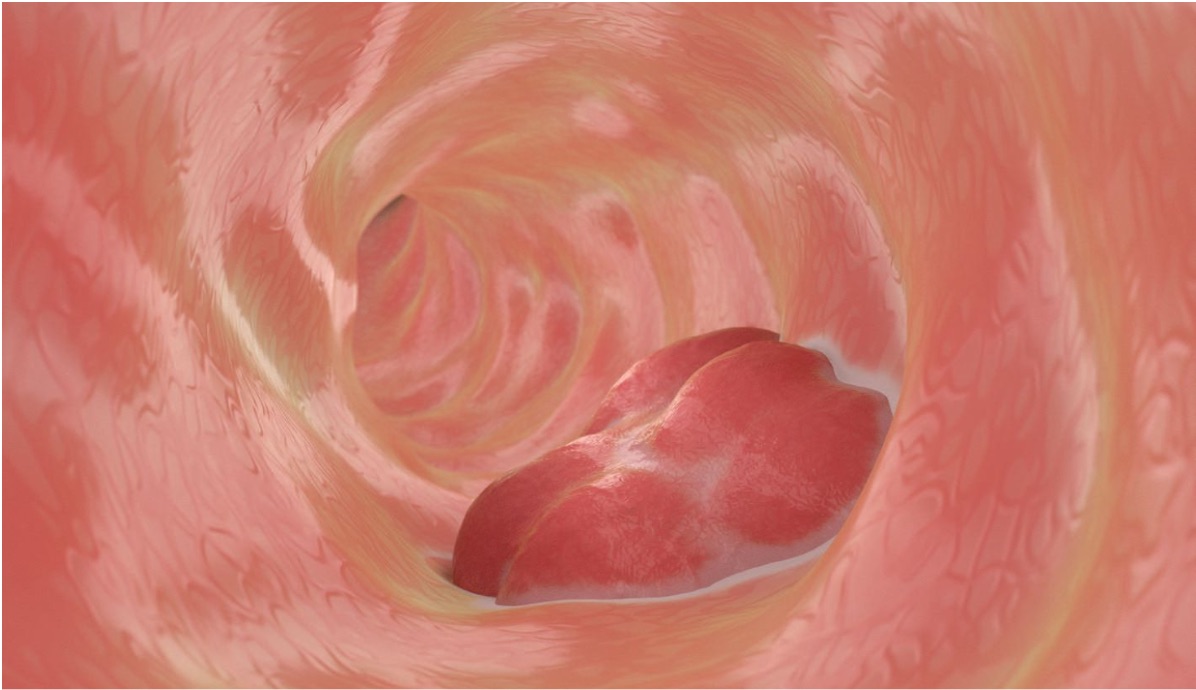
The human gut is a mysterious and complex ecosystem, teeming with trillions of microbes that carry out countless vital functions—fermenting fibers, producing essential vitamins, and communicating with the immune system. But now, scientists are asking these tiny organisms to take on a new, unprecedented role: the detection of cancer. An international research team, led by molecular biologists Robert Cooper and Jeff Hasty from the University of California, San Diego, and bowel cancer experts Josephine Wright, Susan Woods, and Daniel Worthley from South Australia, have engineered a bacterial biosensor capable of identifying a DNA mutation associated with cancer. Published in the journal *Science*, this groundbreaking study offers a glimpse into the potential future of cancer diagnostics. However, numerous questions remain unanswered. How accurate is the bacterial biosensor in detecting early-stage cancer? What happens when these engineered bacteria interact with the diverse and unpredictable microbial population of the gut? Can the gut bacteria distinguish between cancerous and non-cancerous mutations without triggering false alarms? As these questions hang in the air, the researchers are faced with the challenge of refining their technology to ensure it can be used reliably in clinical settings. Will their work pave the way for a revolution in cancer detection, or will these promising new tools prove too volatile for everyday use?
In the realm of scientific innovation, the creation of bacterial biosensors has always been a groundbreaking achievement. While scientists have successfully engineered bacteria to detect general signs of inflammation or bleeding within the gut, this new development introduces a far more intricate concept: a bacterial biosensor capable of detecting specific DNA sequences from the very tissues of the host itself. But how exactly does this unprecedented technology work, and what unforeseen consequences might it have?
To accomplish this feat, researchers turned to *Acinetobacter baylyi*, a bacterium known for its unique ability to uptake extracellular DNA and integrate these foreign sequences into its own genome. This ability, once harnessed, allows the bacteria to act as a highly specialized detector, identifying DNA from host tissues with precision. Yet, despite the promise of this breakthrough, many critical questions remain unanswered.
What are the long-term effects of this process on both the bacteria and the host? Could this engineered bacterium inadvertently trigger immune responses or cause unforeseen genetic mutations? As the research unfolds, scientists grapple with the potential risks of such an invasive and powerful tool. How might this technology change the way we diagnose and treat diseases, and what ethical dilemmas will emerge from the ability to detect genetic material in this new way? The possibilities are both exciting and chilling, leaving everyone wondering how far this technology could go.
David Riglar, a microbiome researcher at Imperial College London, expressed his intrigue at the groundbreaking approach of using living bacteria to sense disease within the gut. "The idea of harnessing naturally competent bacteria to detect DNA changes and then using them as biosensors is incredibly exciting," Riglar remarked, his enthusiasm clear despite not being directly involved in the study. The concept of using bacteria in this manner was, at the time, an ambitious leap into uncharted territory, filled with possibilities but also unknowns.
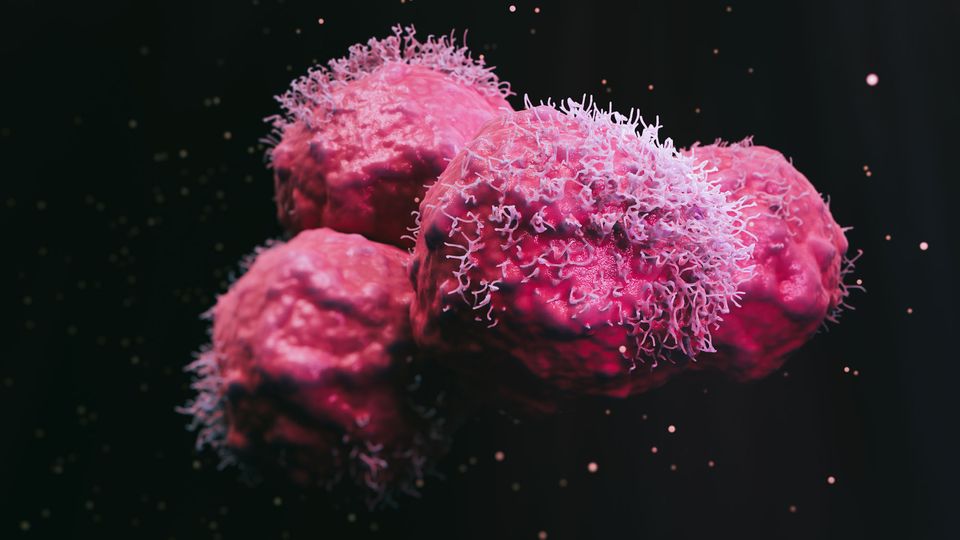
In this particular study, the researchers set out to engineer *A. baylyi*, a strain of bacteria, to detect a mutation in codon 12 of the KRAS gene, a known marker for colorectal cancer. "It seemed almost like science fiction back then," reflected Worthley, one of the researchers. Yet, through collaboration, pooling expertise in synthetic biology, and leveraging animal models of colorectal cancer, the team achieved what initially seemed impossible. But even with this success, several pressing questions lingered: Could this engineered bacteria work consistently within the human gut environment? What other mutations or markers could they target? How would the body’s immune system react to these living biosensors? The team was excited, but they were also cautious, aware of the layers of complexity they were navigating. The deeper they dug into this uncharted frontier, the more questions arose, each one revealing another mystery. What had they really uncovered, and were they ready for the implications? The unknowns were mounting, and the path forward was as thrilling as it was uncertain.
In the early stages of their proof-of-concept experiments, the researchers embarked on a bold and ambitious journey, manipulating both *Acinetobacter baylyi* (A. baylyi) and the tumor organoids they hoped would serve as the foundation for a groundbreaking medical discovery. They started by genetically modifying tumor cells, introducing a functional copy of the antibiotic resistance gene, kanR, flanked by KRAS homology arms. The bacteria, in turn, were engineered to possess matching KRAS homology arms, but with one critical difference: two stop codons that prevented the expression of the kanR gene.
As the experiment unfolded, the bacteria ingested the tumor DNA, the homology arms aligning perfectly with the DNA sequences. This allowed the bacteria to integrate the functional kanR gene into their own genomes, unlocking the possibility of growth on antibiotic-laced plates. But questions loomed. Could this integration process truly work as intended, or was something else at play? Were the bacteria's genomes truly altered in the way the researchers believed? And what about the tumor organoids themselves—could they influence the bacteria in unexpected ways, perhaps introducing risks no one had anticipated? The researchers, though intrigued, found themselves grappling with more uncertainties as they faced each new discovery, unsure whether they were pioneering a new era of medical breakthroughs or unwittingly opening the door to unintended consequences. The deeper they delved, the more layers of mystery they uncovered.
The researchers were determined to create bacteria capable of specifically detecting mutant KRAS, a notorious marker for cancer. Using the bacteria's own CRISPR-Cas machinery, they directed these molecular scissors to target wild-type KRAS, ensuring that the bacteria would destroy any that carried this version of the gene. But the mutant KRAS—found only in cancerous cells—remained untouched. The idea seemed brilliant: any bacteria with wild-type KRAS would be eradicated, while those with mutant KRAS would thrive. Yet, as they progressed, questions began to arise. Was the CRISPR system really as precise as they hoped? Could there be an unknown variant of KRAS that wasn’t being targeted? Could the engineered bacteria somehow be influencing the tumors in unexpected ways?
When the researchers tested the bacteria against colorectal cancer organoids, the results were striking, but troubling. Only the bacteria exposed to organoids with engineered donor DNA developed antibiotic resistance. This anomaly suggested that the engineered bacteria were somehow interacting with the tumors in a way they hadn’t anticipated. Was this resistance a sign of a deeper, more complex biochemical interaction, or was something else at play entirely? What role did the engineered donor DNA have in this unexpected result? The more the researchers delved, the more layers of mystery they uncovered, and the more they realized they were dealing with forces far beyond their initial understanding.
The researchers took their investigation to the next level by testing the biosensors in vivo, administering the engineered bacteria via enema to three distinct groups of mice: those without tumors, those with normal colorectal tumors, and those with the specially engineered colorectal tumors. The results were striking—only the biosensors introduced to the mice with engineered tumors showed growth in the presence of the antibiotic, confirming the hypothesis that the bacteria could act as a signal, indicating the presence of colorectal cancer that had been modified for experimental purposes.
However, this success raised more questions than answers. Why did the bacteria respond only to the engineered tumors and not to the normal colorectal tumors? Was there something inherently different in the engineered tumors that allowed them to interact with the biosensors in such a specific way? How did the presence of the antibiotic influence this reaction, and could other compounds potentially alter the biosensor’s response? The researchers couldn’t ignore the possibility that there were variables they hadn’t accounted for—perhaps something within the gut microbiome, or even the immune system, was affecting the bacteria's behavior.
As they pondered these questions, a sense of unease began to settle among the team. Were they truly in control of the experiment, or was there something hidden, lurking in the depths of their research, waiting to reveal itself in ways they hadn't anticipated? The implications were vast, and with every discovery came new uncertainties.
The initial data had been promising, but there was a glaring issue: human colorectal tumors don’t naturally harbor a perfectly placed antibiotic resistance gene, one that bacteria could simply acquire. This discrepancy led the researchers to re-evaluate their approach. They pivoted, shifting their focus to detecting natural tumor DNA that contained the KRAS mutation—a key alteration linked to various cancers. However, as they adjusted their methods, they faced even more pressing questions. Could this modified strategy truly capture the complexity of tumor behavior, or were they overlooking crucial factors?
In a bid to control the expression of foreign elements within the tumor, the team introduced a repressor gene within the KRAS homology arms. This repressor gene served a dual purpose: it blocked the expression of a downstream kanR gene, a marker used to track bacterial acquisition. Yet, even as this new layer of control was implemented, questions loomed larger. What unforeseen consequences might arise from this genetic manipulation? How would the tumor’s microenvironment respond to this new genetic alteration? Was the kanR gene truly silenced, or could there be a subtle leak that would compromise the entire experiment?
As they continued their work, each step forward seemed to reveal more unknowns. The researchers could sense a growing tension—there were too many unanswered questions, and the looming uncertainty made it difficult to predict whether their strategy would succeed or unravel entirely.
When the bacteria mysteriously swapped their KRAS DNA for the tumor's KRAS, something strange happened. The repressor that typically controlled genetic expression was suddenly lost, setting off a chain reaction that allowed the antibiotic resistance gene to be activated. This was not supposed to happen. The team had assumed the repressor would always remain intact, but now, with it gone, new questions arose. Why did this particular mutation cause the repressor to disappear? What was the real connection between the bacterial and tumor DNA, and how did the bacteria gain access to such specific cancer-associated mutations?
As the CRISPR-Cas system continued to target the wild type KRAS for destruction, the biosensors started behaving in unexpected ways. They became resistant to antibiotics, but only when the cancerous mutation was present. The team had initially assumed the system would only identify normal and mutant KRAS in a straightforward manner, but the results were much more complex. Why did the biosensors react this way, and what did it mean for the broader implications of gene transfer? Could the bacteria be evolving in response to something they hadn’t anticipated?
The team, still in shock, couldn’t stop questioning the implications. They named the technique CATCH—Cellular Assay for Targeted, CRISPR-Discriminated Horizontal Gene Transfer—but the unanswered questions haunted them. Would this discovery lead to new treatments, or was it merely the tip of an even more dangerous iceberg?
Despite their initial progress, Riglar urged a sense of caution. "We’ve made significant strides, but we must not get ahead of ourselves," he warned. "Thinking that these systems are ready for clinical application is premature." His voice held an edge of concern, as if the promise of success was both exhilarating and dangerous in equal measure. "We need to remember, this is far from the endpoint," he emphasized.
Worthley, standing nearby, nodded in agreement, though his expression betrayed a tinge of uncertainty. "Absolutely," he murmured, but his eyes darted over to the data on the screen, where complex algorithms churned out results. The numbers seemed promising, almost too promising. Yet, the unanswered questions hung in the air like a fog. What were they overlooking? How many unknown variables had they yet to encounter?
The room fell into an uneasy silence, as the team struggled to reconcile the excitement of their discoveries with the weight of the unknown. Could their work truly be as revolutionary as they hoped, or were they heading down a path that could lead to unforeseen consequences? How many more layers of complexity would they uncover before they could even consider moving forward? Riglar’s warning had unsettled them all, but no one could deny the gnawing curiosity that kept pushing them forward.
The researchers are in the midst of unraveling the complexities of improving their biosensor's sensitivity to natural tumor DNA, specifically within the unpredictable and hostile environment of the colon. Their current work hinges on an intricate challenge: how can they refine the technology to detect minute traces of mutant KRAS amidst the chaos of the digestive system? The biosensors, designed to work with genetically engineered bacteria, must not only be effective but capable of surviving the rigorous journey through the human digestive tract. This raises further questions: How can these delicate organisms endure the harsh acidic conditions of the stomach, and how will they navigate the ever-changing landscape of gut microbiota?
Compounding the issue, ethical concerns regarding the administration of antibiotic-resistant bacteria to humans loom large. In light of this, researchers are exploring alternative ways to signal the presence of mutant KRAS without relying on these bacteria. What other strategies could replace this risky method? Will they find a viable solution in time?
To make this technology commercially viable, the biosensors must be delivered orally—a daunting task that brings with it more unknowns. How will they survive the acidic stomach environment? How will they relay their findings to researchers once they have navigated the labyrinth of the gut? The answers remain elusive, and the pressure is mounting as the team works tirelessly to crack the code of this life-saving technology.
Worthley envisions a future where biosensor bacteria, engineered with unprecedented precision, could revolutionize healthcare, particularly in remote or low-resource areas like the Australian outback. His belief rests on the groundbreaking concept that, by embedding all the diagnostic sophistication within the bacteria themselves, these microorganisms could serve as reliable point-of-care diagnostics without requiring the advanced equipment typical of modern laboratories. But as promising as this vision is, numerous questions remain unanswered. How will these biosensors respond in environments as harsh and unpredictable as the outback? Will they remain stable in extreme temperatures, or could the bacteria themselves become compromised? The reliability of such a system, especially in a region where access to healthcare is limited, is still a mystery.
Worthley and his team, though confident in their innovation, can't help but wonder: How will local populations react to using these microscopic agents for their health? Will they embrace the technology, or will skepticism arise due to its unfamiliarity? As they prepare to test their biosensor bacteria in the field, they are left grappling with unknowns that extend far beyond the science itself. What other unforeseen challenges might emerge, and will they be able to adapt their groundbreaking technology to meet the needs of the people who need it most?
The researchers, eager to uncover broader applications for their groundbreaking work, begin to consider the far-reaching possibilities, yet their ambitions are shadowed by a veil of uncertainty. What if these engineered bacteria could not only detect tumor DNA but also release a genotype-specific small-molecule therapeutic? The idea of bacteria being able to deliver treatment precisely where it’s needed seems almost too good to be true, but the questions pile up. Could they develop a bacteria strain that responds effectively to specific oncogenic mutations? Could the same bacteria adapt to treat even the most stubborn infections, like Clostridium difficile, without triggering dangerous side effects? While Worthley is enthusiastic about the potential of merging diagnosis and therapy, a sense of unease lingers. How reliable will these engineered bacteria be when faced with the complexity of human biology? What if they malfunction or become resistant over time? Will they truly distinguish between healthy cells and cancerous ones without causing harm? As these questions swirl in the lab, the researchers are left grappling with a sense of anticipation mixed with trepidation. Will their creations be the breakthrough they hope for, or will they uncover new, unanticipated dangers lurking in the microscopic world? The road ahead is full of promise, yet uncertain and fraught with unknowns.























0 Comments