Research led by Stanford Medicine reveals that when the brain struggles to filter incoming information and make predictions about future events, it can lead to psychosis. Within the brains of individuals experiencing psychosis, two critical systems malfunction: one responsible for filtering important external events and internal thoughts, and another comprised of pathways that anticipate rewards. The dysfunction of these systems results in difficulty discerning reality, often leading to hallucinations and delusions. These insights stem from a study led by Stanford Medicine, published on April 11 in Molecular Psychiatry, which analyzed brain scan data from children, adolescents, and young adults with psychosis. The findings validate an existing theory regarding the mechanisms behind breaks with reality. Lead author Kaustubh Supekar, PhD, clinical associate professor of psychiatry and behavioral sciences, notes that this research offers a valuable framework for understanding the development and progression of schizophrenia, a complex condition.
The findings, observed in individuals with a rare genetic disease called 22q11.2 deletion syndrome who experience psychosis as well as in those with psychosis of unknown origin, advance scientists’ understanding of the underlying brain mechanisms and theoretical frameworks related to psychosis.
During psychosis, patients experience hallucinations, such as hearing voices, and hold delusional beliefs, such as thinking that people who are not real exist. Psychosis can occur on its own and isa hallmark of certain serious mental illnesses, including bipolar disorder and schizophrenia. Schizophrenia is also characterized by social withdrawal, disorganized thinking and speech, and a reduction in energy and motivation.
It is challenging to study how schizophrenia begins in the brain. The condition usually emerges in teens or young adults, most of whom soon begin taking antipsychotic medications to ease their symptoms. When researchers analyze brain scans from people with established schizophrenia, they cannot distinguish the effects of the disease from the effects of the medications. They also do not know how schizophrenia changes the brain as the disease progresses.
To get an early view of the disease process, the Stanford Medicine team studied young people aged 6 to 39 with 22q11.2 deletion syndrome, a genetic condition with a 30% risk for psychosis, schizophrenia or both.
The discoveries, observed in individuals afflicted by a rare genetic condition known as 22q11.2 deletion syndrome, who manifest psychosis, as well as in those with psychosis of uncertain etiology, enhance scientists’ comprehension of the fundamental brain mechanisms and theoretical constructs associated with psychosis.
 // Cras eget sem nec dui volutpat ultrices.
// Cras eget sem nec dui volutpat ultrices.
During episodes of psychosis, patients undergo hallucinations, such as auditory perceptions, and maintain delusional convictions, such as believing in the existence of non-existent individuals. Psychosis can manifest independently and is a characteristic feature of certain severe mental disorders, including bipolar disorder and schizophrenia. Schizophrenia is further characterized by social withdrawal, disorganized thought and speech patterns, and a decline in both energy and motivation.
Understanding the onset of schizophrenia in the brain poses significant challenges. Typically emerging during adolescence or early adulthood, most individuals affected soon initiate antipsychotic medication to alleviate symptoms. When examining brain scans of individuals diagnosed with established schizophrenia, researchers encounter difficulty distinguishing between the impacts of the illness and those of the prescribed medications. Moreover, the alterations in the brain that occur as schizophrenia progresses remain largely unknown.
To gain early insights into the progression of the disease, the Stanford Medicine team conducted a study involving individuals aged 6 to 39 affected by 22q11.2 deletion syndrome, a genetic condition associated with a 30% risk of developing psychosis, schizophrenia, or both.
They discovered that the brain function in individuals with psychosis associated with 22q11.2 deletion syndrome mirrors that of those with psychosis of unknown origin. These brain patterns align with the researchers' previous theories regarding the underlying causes of psychosis symptoms.
Vinod Menon, PhD, the senior author of the study and the Rachael L. and Walter F. Nichols, MD, Professor, along with being a professor of psychiatry and behavioral sciences and the director of the Stanford Cognitive and Systems Neuroscience Laboratory, stated, "The brain patterns we identified validate our theoretical frameworks concerning the malfunctioning of cognitive control systems in psychosis."
He further explained that thoughts detached from reality can hijack the brain's cognitive control networks, disrupting their normal operation. This disruption enables intrusive thoughts to take precedence, resulting in symptoms characteristic of psychosis.
Cognitive Filtering Mechanism
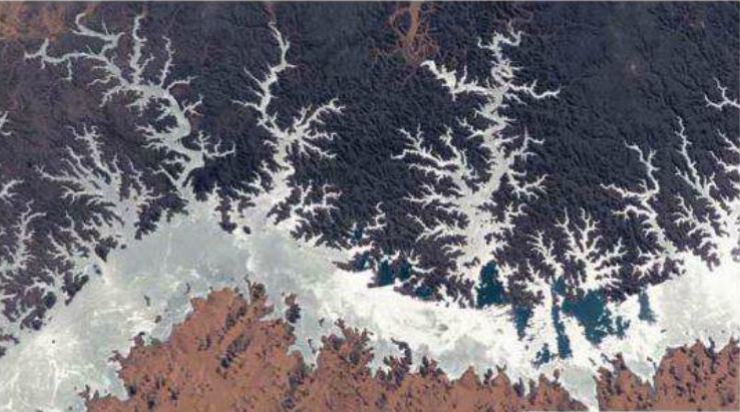
Ordinarily, the brain operates a cognitive filtering mechanism, often referred to as the salience network, which functions covertly to selectively guide our attention towards significant internal thoughts and external stimuli. This mechanism aids in disregarding irrational thoughts and insignificant occurrences, enabling us to focus on tangible and meaningful aspects of our surroundings, such as navigating traffic to prevent accidents.
The ventral striatum, a small brain region, along with associated dopamine-driven pathways, plays a pivotal role in anticipating rewarding or noteworthy stimuli.
In this study, researchers compiled functional MRI brain-scan data from a cohort of young individuals diagnosed with 22q11.2 deletion syndrome, comprising 101 participants scanned across three different academic institutions. (The study also encompassed brain scans from several comparison groups not affected by 22q11.2 deletion syndrome: 120 individuals with early idiopathic psychosis, 101 with autism, 123 with attention deficit/hyperactivity disorder, and 411 healthy controls.)
This genetic disorder, characterized by the deletion of a segment of the 22nd chromosome, affects approximately 1 in every 2,000 to 4,000 individuals. Alongside the 30% susceptibility to schizophrenia or psychosis, individuals with this syndrome may also manifest autism or attention deficit hyperactivity disorder, hence the inclusion of these conditions in the comparison groups.
 // Cras eget sem nec dui volutpat ultrices.
// Cras eget sem nec dui volutpat ultrices.
The researchers employed a spatiotemporal deep neural network, a form of machine learning algorithm, to delineate patterns of brain function among all individuals with 22q11.2 deletion syndrome compared to healthy counterparts. Leveraging a subset of patients whose brain scans originated from the University of California, Los Angeles, they developed an algorithmic model capable of distinguishing between brain scans of individuals with and without 22q11.2 deletion syndrome, achieving a prediction accuracy exceeding 94%. Subsequently, they validated the model across additional cohorts of individuals with or without the genetic syndrome who had undergone brain scans at UC Davis and Pontificia Universidad Católica de Chile, demonstrating sorting accuracy ranging from 84% to 90% in these independent samples.
The researchers then utilized the model to explore the predominant brain features associated with psychosis. Previous studies on psychosis yielded inconsistent results, likely due to inadequate sample sizes.
By comparing brain scans of individuals with and without psychosis within the 22q11.2 deletion syndrome, the researchers identified the anterior insula and ventral striatum as the primary contributors to psychosis. This observation held true across different patient cohorts.
Furthermore, when comparing the brain characteristics of individuals with 22q11.2 deletion syndrome and psychosis to those with psychosis of unknown origin, the model revealed significant overlap, suggesting that these brain features are common to psychosis in general.
A second mathematical model, trained to distinguish between subjects with 22q11.2 deletion syndrome and psychosis and those with the genetic syndrome but without psychosis, achieved 77.5% accuracy in identifying brain scans from individuals with idiopathic psychosis. This finding underscores the importance of the brain's filtering and predictive mechanisms in psychosis.
Moreover, this model specifically targeted psychosis and was unable to classify individuals with idiopathic autism or ADHD.
Menon expressed excitement in connecting their research back to the fundamental question of identifying dysfunctional brain systems in schizophrenia. The discovery of similar patterns in the context of 22q11.2 deletion syndrome underscores the consistency of brain signatures in psychosis. However, these signatures were not evident in individuals with the genetic syndrome but no psychosis, hinting at future research avenues.
Applications for treatment or prevention
Furthermore, by aligning with the scientists' theory on the genesis of psychosis, the findings carry significant implications for comprehending the condition and potentially averting its onset.
Supekar expressed his aspiration to forestall or postpone the onset of schizophrenia, highlighting that the congruence between the new findings and their previous research hints at potential avenues for prevention. He emphasized the challenge posed by diagnosing schizophrenia due to the considerable brain damage already incurred by that time.
Early anomalies in functional interactions among brain regions within the same systems were observed, indicating that these abnormalities manifest as early as childhood rather than emerging solely in adulthood.
These revelations underscore the necessity of approaching individuals with psychosis with empathy. The researchers intend to explore the efficacy of existing treatments like transcranial magnetic stimulation or focused ultrasound, targeting specific brain centers in young individuals at risk of psychosis, such as those with 22q11.2 deletion syndrome or a familial history of schizophrenia, to assess their potential in either delaying onset, mitigating symptoms, or both.
The findings also imply that utilizing functional MRI to observe brain activity at critical centers could aid researchers in probing the effectiveness of current antipsychotic medications.
Although it remains perplexing why individuals experience detachment from reality, given its evident risks to well-being, understanding the "how" is now within grasp, according to Supekar. "From a mechanistic standpoint, it aligns logically," he remarked.
Menon emphasized the significance of approaching individuals with psychosis with compassion, expressing hope that their research not only advances scientific comprehension but also fosters a cultural shift towards empathy and support for those grappling with psychosis.
"I recently had the opportunity to interact with members of our department's early psychosis treatment cohort," he recounted. "Their message was poignant and resounding: 'We share more commonalities than disparities. Like everyone else, we navigate our own peaks and valleys.' Their words resonated as a heartfelt plea for increased empathy and comprehension towards those confronting this condition, urging for a perspective of empathy and solidarity."
Contributors to the study hailed from UCLA, Clinica Alemana Universidad del Desarrollo, Pontificia Universidad Católica de Chile, the University of Oxford, and UC Davis.
The research was financially supported by the Stanford Maternal and Child Health Research Institute's Uytengsu-Hamilton 22q11 Neuropsychiatry Research Program, FONDEYCT (the National Fund for Scientific and Technological Development of the government of Chile), ANID-Chile (the Chilean National Agency for Research and Development), and the U.S. National Institutes of Health (grants AG072114, MH121069, MH085953, and MH101779).




















0 Comments